Level 1A evidence for the efficacy of endovascular treatment (EVT) was established in 2015 after the positive results of several randomized clinical trials. [1,2] This evidence concerned large vessel occlusions (LVOs), i.e. the intracranial internal carotid artery and first segment of the middle cerebral artery. Furthermore, the 2015 guideline stated that ‘patients should receive endovascular therapy with a stentretriever’ [3].
Since then, experience, developments and new insights have changed the perspective on EVT.
Thrombectomy with aspiration
Aspiration as a technique to remove the clot from an intracranial artery was already used before the success of stentretriever thrombectomy was shown with overwhelming evidence in several trials [4].
The first randomized controlled trial investigating the efficacy of clot aspiration in the setting of acute ischemic stroke was halted after the publication of the positive thrombectomy trials using mainly or exclusively strentretriever [5]. Unfortunately, they could not confirm efficacy: a signal towards effect was seen, but numbers were too small for statistical significance. Later studies supported the positive signal seen in this first trial and a randomized trial confirmed non-inferiority of aspiration as primary EVT technique compared with stent retriever EVT [6]. Moreover, they showed that EVT with aspiration as first choice is less costly than starting with a stentretriever, even when a considerable part of the aspiration first group needs conversion to stentretriever EVT after failure of aspiration. All these trials concerned LVOs in the anterior circulation and the at that time available aspiration catheters were accustomed to these vessels taking into account that larger bore catheters go with higher aspiration force [7].
Thrombectomy in medium vessel occlusions
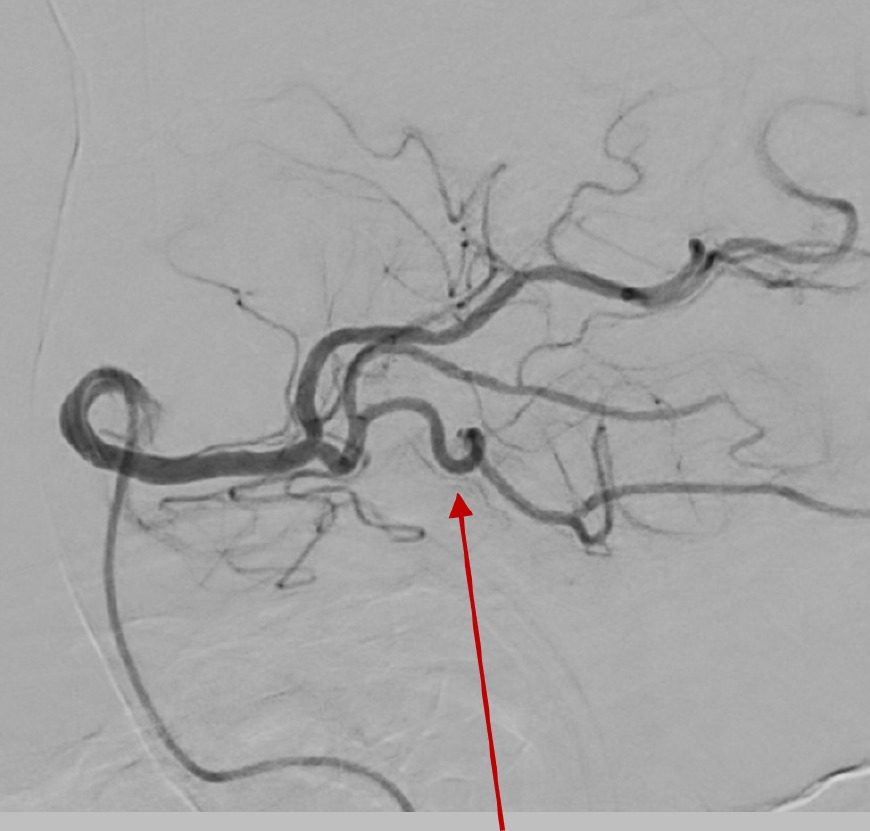
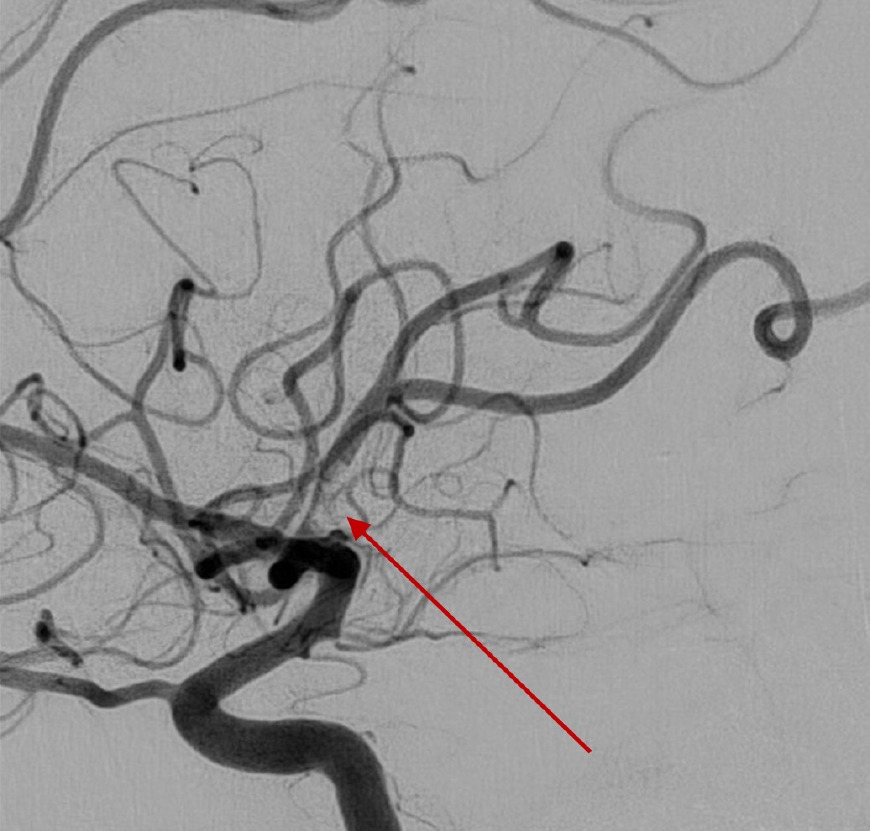
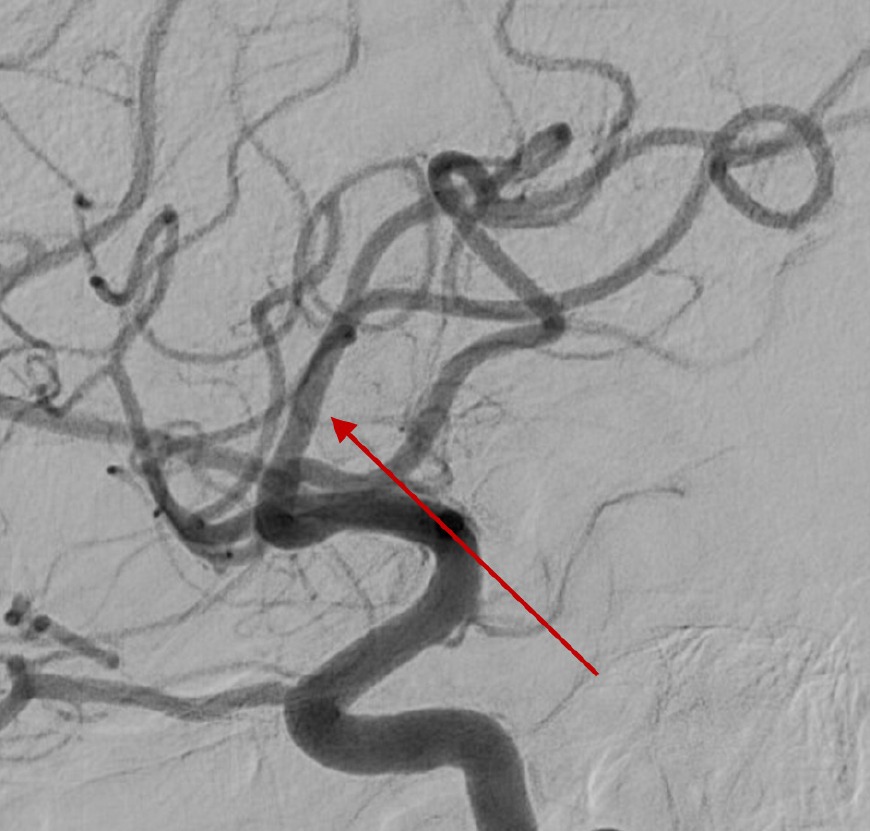
Medium vessel occlusions (MeVOs) usually comprise the M2 and M3 segments of the middle cerebral artery, as well as the A2 and A3 and P2 and P3 from the anterior and posterior cerebral arteries. The diameters are smaller than the LVOs and the area affected is smaller which theoretically results in less severe symptoms. With a reported incidence of 16 per 100.000 patient/year and -although less severe- not neglectable neurological symptoms, these MeVOs require adequate acute treatment [8,9].
Despite milder neurological symptoms at presentation, these patients may have poor clinical outcomes if not treated. Excellent functional outcome (mRS 0-1) is only achieved in 50% of patients and, while the recanalization rate after intravenous thrombolysis (IVT) is higher in MeVOs than in LVOs, still fewer than half of MeVOs treated with IVT achieve early recanalization, which is strongly associated with better clinical outcomes [8]. Following the success of EVT in LVOs, it was a logical step to explore its benefit in MeVOs as well. Smaller stentretrievers and aspiration catheters, dedicated for more distal vessels, appeared to facilitate EVT in MeVOs. However, because of a higher risk of complications, mainly vessel perforations in combination with generally milder symptoms and higher recanalization rates of IVT than in EVT for LVOs, it remained unclear whether EVT would benefit patients with MeVO strokes [10]. Several randomized trials are currently ongoing to provide insight if – or which – MeVO stroke patients may benefit from EVT. Most of these trials mandate use of a stentretriever. However, some leave the treatment technique to the discretion of the treating physician, allowing aspiration as first choice.
Thrombectomy with aspiration in medium vessel occlusions
Despite lacking evidence of EVT in MeVO strokes, some publications have already appeared on the comparison between aspiration and stentretriever technique for EVT in more distal vessels [11-15]. Three of these studies showed a slight benefit for using aspiration as first attempt [11,13,15], while the other two did not see a difference in outcomes. One study, from 2017, which found no difference in clinical outcomes noted better technical results (less emboli and higher reperfusion rates) with aspiration [14].
The ongoing trials on EVT in MeVOs may shed a light on efficacy of both techniques. With the aforementioned lower costs associated with aspiration as a frontline thrombectomy technique, equal clinical results may lead to a preference for aspiration. Until the results of those trials are made public, choice of technique will depend on personal preferences of treating physicians.